- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 0
- 1
- 2
- 3
- 4
- 5
- ,
- 0
- 1
- 2
- 3
- 4
- 0
- 1
- 0
- ,
- 0
- 0
- 0
In 2012, the prevalence of HIV was approximately 30 times higher among men how have sex with men (MSM) and Black African men and women than in the general population. Sexual behaviours, infections acquired abroad, migration and HIV related stigma and discrimination contribute to this disparity.
-MIGRANT POPULATIONS
MIGRANT POPULATIONS
AND HIV
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- .
- 0
- 1
- 2
- 3
- 4
- 5
- M
- i
- l
- l
- i
- o
- n
- 0
- 1
- 2
- 3
- 4
- 0
- ,
- 0
- 1
- 2
- 0
- 1
- 2
- 3
- 4
- 5
- 0
- 1
- U
- n
- k
- n
- o
- w
- n
- U
- n
- k
- n
- o
- w
- n
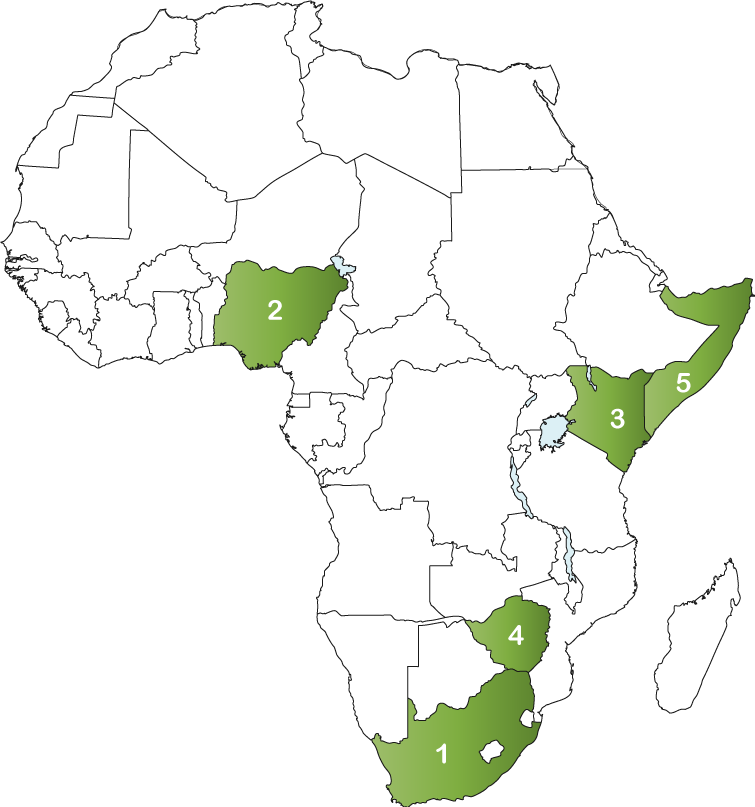
TOP 5 AFRICAN COUNTRIES
OF ORIGIN FOR MIGRANTS IN UNITED KINGDOM
- 1. South Africa: 218,732
- 2. Nigeria: 216,268
- 3. Kenya: 151,053
- 4. Zimbabwe: 132,942
- 5. Somalia: 110,775
-TOTAL POPULATION
PEOPLE LIVING WITH HIV
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- ,
- 0
- 1
- 2
- 3
- 4
- 0
- 0
NEW INFECTIONS
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- ,
- 0
- 1
- 2
- 3
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 0
HIV TREATMENT CASCADE
KEY AND AFFECTED POPULATIONS
29% new diagnoses in U.K. among people born in Africa
52% of new diagnoses
Men who have sex with men are the most group most affected by HIV in the UK. IN 2012, there were an estimated 41,000 men who have sex with men living with HIV of whom 7,300 (18%) were unaware of their infection. An estimated 2,400 men who have sex with men acquired HIV each year over the past 10 years. New diagnoses among men who have sex with men reached an all-time high in 2012 with 3,250 infections. The increase in numbers may be the result of both high levels of HIV transmission and an increase in HIV testing. Among men who have sex with men, the number of late HIV diagnoses reduced from 42% to 34% in 2012.
Black African men and women were the second largest group affected by HIV in 2012 with 31,800 people living with HIV. 11,100 Black African men and 20,700 Black African women were living with HIV in 2012. 23% of Black African men and women were unaware of their infection in 2012. An estimated 1,000 Black African men and women acquired HIV annually over the past 5 years.
Sex workers are not a well-studied group in the United Kingdom although they are assumed to be at an increased risk of sexually transmitted infections including HIV. A 2011 study on the sexual health of female sex works compared with other women in England revealed that overall, female sex workers in England have access to high-quality sexual health care through genitourinary medicine clinics. There was evidence of geographical inequality in access to services however. Though uptake of HIV testing was generally high through these clinics, a minority of female sex workers did not appear to access HIV testing. Barriers to uptake were not identified. It was found that the study population was predominately migrant women. Differences in service usage among migrant female sex workers was found and may indicate that migrant female sex workers experience unmet needs for primary care services. The study found that there was little variation in the sexual health outcomes among female sex workers by migrant status.
1% of new diagnoses
An estimated 2,200 injection drug users were living with HIV in 2012, of whom 300 were unaware of their infection. As of 2012, HIV transmission among this group was on-going, although at a low level.
HEALTH
Britain’s Black population began to grow in the 1940’s to 1960’s with the arrival of Caribbeans. In the 1980’s wealthy Nigerians and Ghanaians along with rural migrants and refugees from Somalia and Zimbabwe began to settle in Britain. As of 2016, Britain’s Black population constitutes 3% of the population or 2 million Black Africans and Black Caribbeans.
Between 1993 and 2015, the foreign born population in the United Kingdom more than doubled from 3.8 million to approximately 8.5 million people. People migrate to the United Kingdom for a number of reasons including economic migration, family reunification, to study and to seek asylum. Many migrants arrive relatively healthy in the United Kingdom but their health can deteriorate over time. Asylum seekers and refuges in the United Kingdom experience higher rates of depression and anxiety than the national population and other migrants.
The United Kingdom’s health care system is publicly funded and coverage is universal. All those considered ‘ordinarily resident’ are entitled to health care that is largely free. ‘Ordinary residence’ means a person living in the United Kingdom on a lawful, voluntary and properly settled basis. The National Health Service (NHS) provides coverage for inpatient and outpatient (ambulatory) hospital (specialist) care; physician (general practitioner) services; inpatient and outpatient drugs; dental care; mental health care; learning disabilities; and rehabilitation. Drugs prescribed by a general practitioner are subject to a co-payment although about 88% of drugs are exempt from charges.
Entitlements to the NHS are based on immigration status. Migrants who have been living in the United Kingdom “legally” for 12 months, permanent residents, and students who have been in the United Kingdom for more than 6 months, individuals from countries with a reciprocal agreement, refugees and asylum seekers are entitled to full NHS treatment. Asylum seekers are only eligible for access to free health care services if they have submitted an application to remain in the United Kingdom. If their application for asylum is rejected, their eligibility for access to health care is taken away.
In 2011, there were approximately 400,000 undocumented migrants living in the United Kingdom. Undocumented migrants are provided emergency care, treatment for illnesses that threaten public health (HIV, tuberculosis or malaria, for example), contraception and compulsory psychiatric treatment. Some undocumented migrants may have access to primary care providers, although this is inconsistent. Undocumented migrants and asylum seekers whose applications have been rejected can access health care through the private health insurance market although many do not have the means to do this. As a result the only care they are entitled to is emergency care.
Barriers to health care access include inadequate information, insufficient support in interpreting and translating for those who do not speak English, lack of access to reliable transport, confusion around entitlement to some types of health care services especially for undocumented migrants.
Other barriers include lack of knowledge on health service entitlements for migrants by health service providers as well as cultural insensitivity by front line health care providers.
In 2012, HIV treatment was made free to anyone with HIV in the United Kingdom. In 2014, 91% of people living with HIV (85, 489 people) were on antiretroviral treatment (ART). The United Kingdom has met two of UNAIDS 90-90-90 targets. Although ART coverage is high among Black Africans (92%), one study found that one third Black Africans living with HIV in the United Kingdom have been discriminated against because of their HIV status and half have been discriminated against by health care workers. Undocumented migrants have encountered difficulties in finding a primary care physician and are often required to provide proof of identity, which may act as a deterrent in seeking care. Additionally, many migrants do not understand the NHS eligibility for care and do not know how to apply for treatment.
HIV disproportionately affects Black African men and women in the United Kingdom. While Black Africans make up 1.8% of the United Kingdom’s population, they accounted for 34% of all HIV diagnoses in 2012. Additionally, in 2012, 68% of Black African men and 61% of Black African women were diagnosed late with HIV. Late diagnoses can reduce the benefits of HIV treatment and reduce life expectancy. The high levels of poverty, unemployment and poor housing faced by Black Africans in the United Kingdom increase the risk of HIV susceptibility.
The United Kingdom’s immigration system affects the physical and mental health of Black African men and women in the United Kingdom. Although access to HIV treatment is free for everyone in the United Kingdom, other NHS health services are restricted.
POLICY
Although the United Kingdom provides universal coverage for health care to citizens and some other groups of migrants, inequities still exist with regard to access to health care and outcomes in health. Poor access to health care and poor patient outcomes are strongly associated with social disadvantage in the United Kingdom. In 2011/12, social inequality was associated with less primary care supply and quality.
One third of Black Africans living with HIV in the United Kingdom have been discriminated against because of their HIV status and half had been discriminated against by health care workers. Given that Black Africans are disproportionately affected by HIV and face increased stigma and discrimination as well as barriers to accessing necessary health care services, policies must be enacted that target the reduction of barriers to health care access for this group.
Although there has been a decline in diagnoses of HIV among Black African men and women in the United Kingdom in recent years, there is consensus that the reduction in HIV diagnoses is the result of a decline in migration from sub-Saharan African to the United Kingdom (stricter visa requirements were imposed for people from Zimbabwe, for example). 9 The proportion of Black African men and women acquiring HIV in the United Kingdom has been on the rise.
Black African men and women in the United Kingdom generally have a higher level of education than the national average but are more likely to be unemployed or in low paying work. 8 Black African people living with HIV are seriously affected by poverty in the United Kingdom. Additionally living with HIV can impact a person’s ability to work and their employment opportunities and may lead to financial difficulties and challenges such as residential status.
Public anxiety about migration to the United Kingdom has been on the rise since the 1990’s. Policy makers in the United Kingdom have developed policies to attempt to manage migration by implementing a Points-Based System for Migration for example. However managing migration and meeting labour market demands in the United Kingdom has proved to be difficult. Living with HIV can impact a person’s ability to work and their employment opportunities and may lead to financial difficulties and challenges such as residential status.
Health, labour and immigration policies are often developed in sector siloes. Given that Black Africans are more likely to be unemployed or in low paying work and experience higher acquisition of HIV, along with more difficulty navigating and accessing the health care system, integrating policies to alleviate poor health outcomes and increase labour market participation must be developed.
THE RESPONSE
In the United Kingdom, men who have sex with men (MSM) and heterosexual Black African men and women are the two groups most affected by HIV. There is a lack of research into the experiences of Black African MSM. An evidence base on Black African MSM and their needs is necessary to develop targeted screening, education and prevention programs.
As of 2014, 40,251 Black African men and women were diagnosed with HIV in the United Kingdom. Policies as well as health and social support programs aimed at Black African women with HIV need to be developed as they face specific needs including reproductive health rights and addressing gender-based violence. Additionally, better experience for Black African women is needed at the point of HIV diagnosis.
In 2012, 68% of Black African men and 61% of Black African women were diagnosed late with HIV. More targeted screening programs are necessary for this groups since late diagnosis can reduce the benefits of HIV treatment and reduce life expectancy.
Founded in 2002, the Global Fund is a partnership between governments, civil society, the private sector and people affected by AIDS, malaria and tuberculosis. The Global Fund raises and invests nearly US$4 billion a year to support programs run by local experts in countries and communities most in need.
Each implementing country establishes a national committee, or Country Coordinating Mechanism, to submit requests for funding on behalf of the entire country, and to oversee implementation once the request has become a signed grant. Country Coordinating Mechanisms include representatives of every sector involved in the response to the diseases.
South African migrants represent the highest migrant group in United Kingdom. Please click here for South Africa’s Country Coordinating Mechanism.
-SOURCES
- http://www.economist.com/news/britain/21689606-mainly-caribbean-community-has-become-mainly-african-oneand-poised-become-more
- http://www.migrationobservatory.ox.ac.uk/resources/briefings/migrants-in-the-uk-an-overview/
- http://jech.bmj.com/content/early/2016/01/12/jech-2015-206742
- http://www.datadictionary.nhs.uk/data_dictionary/nhs_business_definitions/o/ordinarily_resident_de.asp?shownav=1
- http://www.commonwealthfund.org/usr_doc/UK_Country_Profile_2008.pdf
- http://web.stanford.edu/group/sjph/cgi-bin/sjphsite/immigrants-and-barriers-to-healthcare-comparing-policies-in-the-united-states-and-the-united-kingdom/
- https://www.avert.org/professionals/hiv-around-world/western-central-europe-north-america/uk
- http://www.nat.org.uk/sites/default/files/publications/NAT-African-Communities-Report-June-2014-FINAL.pdf
- http://www.unaids.org/sites/default/files/country/documents//GBR_narrative_report_2014.pdf
- http://www.worldometers.info/world-population/uk-population/
- https://www.iom.int/world-migration
- http://sti.bmj.com/content/early/2014/02/03/sextrans-2013-051381.full
- https://www.avert.org/professionals/hiv-around-world/western-central-europe-north-america/uk