- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 0
- 1
- 2
- 3
- 4
- ,
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 0
- 0
- ,
- 0
- 0
- 0
Men who have sex with men and foreign born heterosexuals (of which 75% were born in sub-Saharan Africa) remain the two most affected groups by HIV in France and represented 42% and 38% of HIV diagnoses in 2012. The incidence of HIV in all other groups of people has stabilized in France with the exception of men who have sex with men.
-MIGRANT POPULATIONS
MIGRANT POPULATIONS
AND HIV
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- .
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- M
- i
- l
- l
- i
- o
- n
- U
- n
- k
- n
- o
- w
- n
- U
- n
- k
- n
- o
- w
- n
- U
- n
- k
- n
- o
- w
- n
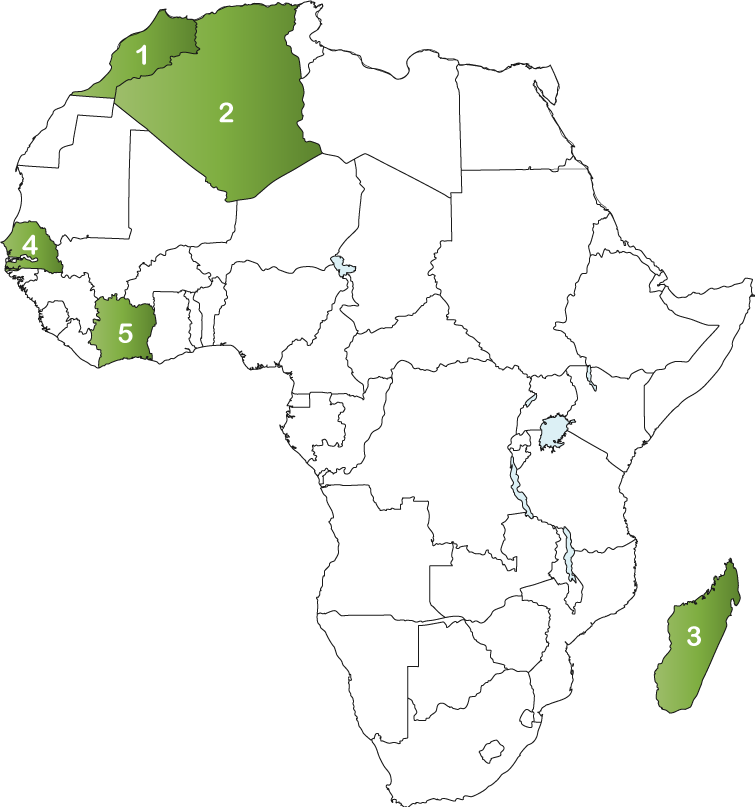
TOP 5 AFRICAN COUNTRIES
OF ORIGIN FOR MIGRANTS IN FRANCE
- 1. Algeria: 1,430,656
- 2. Morocco: 926,466
- 3. Madagascar: 120,400
- 4. Senegal: 117,870
- 5. Ivory Coast: 89,937
-TOTAL POPULATIONS
PEOPLE LIVING WITH HIV
- 0
- 1
- 0
- 1
- 2
- 3
- 4
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- ,
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 0
- 0
NEW INFECTIONS
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- ,
- 0
- 1
- 2
- 3
- 4
- 0
- 0
HIV TREATMENT CASCADE
KEY AND AFFECTED POPULATIONS
42% of new diagnoses in France
42% of new infections
In 2012, 42% of new HIV diagnoses were in MSM. Overall, in 2012, MSM continued to be the population most affected by HIV in the country, accounting for 42% of new diagnosis, this was compared to heterosexuals born in France and persons who use drugs accounting for 17% and 1% of new cases in the same year, respectively. HIV diagnoses in migrant men who have sex with men increased from 1927 men in 2007 to 2459 men in 2012.
1% of new diagnoses
HIV incidence among injection drug users in France remains low. In 2012, a total of 80 injection drug users were diagnosed with HIV, 90% of who were men. Of the injection drug users diagnosed in 2012, 51% were foreign born (mainly from East and Central Europe). Seventy-nine percent of injection drug users in France are men, one in five are homeless and 79% are not employed.
HEALTH
France has a long history of migration. The number of migrants to France has grown from 1.1 million at the start of the 20th century to 7.8 million, or 12% of France’s population in 2015. In 2012, 43% of migrants, or 2.5 million people, were born in Africa. In 2012, there were an estimated 400,000 undocumented migrants in France mainly from Asia, Central Africa, West Africa, Algeria, Morocco, Turkey, and Chechnya.
Studies show that while migrants’ health status was generally better than non-migrants during the 1990s and 2000s, it has been on the decline since. The “healthy migrant effect”, which is largely a result of selective factors for immigration so that mostly healthy migrants immigrate, disappears as the duration of residence increases. Health status for first-generation and female migrants appears to be worse now than it was in the early 2000s.
Migrants in France experience lower use of medical services compared to non-migrants. This inequality can largely be explained by disadvantaged social and economic conditions that migrants in France face. Migration can include a loss of social network and may increase social isolation which may generate obstacles to accessing health care services. Language difficulties among migrants in France has resulted in misunderstanding of health information related to preventive care, to treatment or more broadly to access to healthcare. Discriminatory practices have resulted in one third of beneficiaries from the State Medical Assistance to be refused care form a health professional. Additionally, high levels of unemployment, poverty, low social status and social inequalities act as barriers to migrants receiving HIV specific services in France.
France introduced universal medical coverage for all residents in 2000. Residents in France receive coverage for healthcare services through their employer, as a benefit (for those who are unemployed) or through being a student or retired person. France covers health care costs for those who fall outside the groups who are covered for health care (these are typically undocumented migrants which comprise 0.4% of the population). Health care services covered include primary care, specialist care, hospital care, some dental care and pharmaceutical care (a co-pay is required for most services).
Although the French health care system is generally considered to be of high quality, there are persistent issues with regard to access to care for some. Economically insecure people in France, of which migrants are a key population, experience access issues to primary care. This is likely due to the co-pay that is required to be paid for all health care services. This often results in lack of uptake for treatment for various illnesses.
Over 20% of migrants do not have the optional health insurance that covers the co-pay for health care services. The state generally covers 70% and the health care user is expected to pay the remaining amount. Most employed people, unemployed people, students, and retired people receive additional coverage as a result of their status and therefore are not required to pay the co-pay.
There is a distinction between documented and undocumented migrants when it comes to health care coverage. Documented migrants can claim common law benefits whereas undocumented migrants are only eligible for a specific health care benefit called the State Medical Assistance (SMA). When universal health coverage was introduced for all residents of France in 2000, the SMA was created as health protection for undocumented migrants. The SMA has been the object of intense debate due to claims of perceived fraud and the legitimacy of providing social protection to undocumented migrants. As a result, the SMA has introduced conditions of residence (an undocumented migrant must prove residency for at least 3 months) and some financial contribution to address the criticisms of the program. IF a migrant cannot justify minimum residency, a contingency measure exists where emergency care is covered and treatment to avoid the spread of disease is also covered.
Undocumented migrants can apply for the SMA at various health and social service centres, hospital and non-governmental organizations. Undocumented migrants must provide identification document (e.g., passport, birth certificate, or expired residency permit), an address, evidence of in-country residence for at least three months, and proof that household income is under the threshold (€631/ month as of 2009). The SMA current covers all medical treatment resulting from illness or childbirth within. All healthcare professionals in France are obliged to accept SMA beneficiaries (undocumented migrants). The period of SMA entitlement is one renewable year.
An estimated 180,000 undocumented migrants receive SMA coverage. Undocumented migrants who do not meet SMA eligibility requirements are entitled to: care in life-threatening situations; treatment of contagious diseases, but not other chronic diseases; all types of health care for children; maternity care; and abortion for medical reasons.
Even with the SMA, undocumented migrants face many difficulties in accessing care. Thousands of undocumented migrants do not have SMA, though they appear to be entitled. Main reasons include uneven interpretation and implementation of the law across agencies and cities, lack of awareness of the program, and lack of acceptable identification documents or adequate evidence regarding residency requirements. Additionally, some doctors and pharmacies reportedly refuse to serve people with SMA coverage.
Ethnic minorities and migrants in France experience barriers in accessing HIV services because of high levels of unemployment, poverty, low social status and inequalities. Low socio-economic status among persons from sub-Saharan Africa may often interplay with HIV service-seeking behaviour. Data has shown that women living with HIV who were born in sub-Saharan Africa receive minimal HIV education, with a significant number also confronted with homelessness.
In 2013, France adopted a new national HIV policy where all people living with HIV are offered anti-retroviral therapy and the promotion of a “combined prevention” which links behavioral measures, testing strategies and antiretroviral therapy. Although access to HIV treatment is universal, barriers to access may still exist. These include difficulty in navigating the health care system and being denied care and treatment as a result of discrimination. France also has a higher proportion of delayed HIV diagnosis in migrants, which are likely the result of barriers to accessing health care including stigma, lack of community support, isolation, racism and double discrimination for being an HIV-positive migrant.
POLICY
Although France has a universal health care system with pharmacare coverage, documented and undocumented migrants still experience barriers to accessing health care services as a result of discrimination, stigma, isolation and difficulty in navigating the health care system. Undocumented migrants face difficulty in accessing the state’s publicly funded health care services as identification documents (e.g., passport, birth certificate, or expired residency permit), an address, evidence of in-country residence for at least three months, and proof that household income is under the threshold for receiving state sponsored benefits must be provided. For homeless migrants this would be difficult to do. Additionally, undocumented migrants and HIV-positive migrants may be fearful of presenting themselves at government agencies to register for heath care coverage for fear of deportation.
Given that France provides health care coverage to all residents, irrespective of status, removing the need for providing identification and evidence of in-country residence would remove obstacles for undocumented migrants to access France’s health care system.
France’s labour market can be difficult for new migrants to secure safe and fair employment. Restrictions on foreign nationals working in the public sector and stringent requirements for some jobs can exclude migrants from jobs. New migrants can be excluded from getting jobs in the public sector for example due to restrictions on foreign national. Migrants who arrived in France in 2000 and onwards tended to fare badly in the first few years after arrival. After 9 years in France, most migrants’ labour market performance is similar to that of French nationals. However, unemployment rates for the same group of migrants was 10% lower than native workers in 2011, pointing to persistent structural obstacles to labour market access for migrants.
Migrants’ region of origin, level of education, reason for migration and gender are all factors that are related to how successful they might be at securing safe fair employment. Newly arrived migrants from North Africa and sub-Saharan Africa tend to cluster in low skilled jobs across most sectors of employment. This group tended to have higher credentials than were required for the jobs they were performing.
France has larger proportions of family-driven migration than labour migration. Since some migrants have not been selected on the basis of their skills, they can be at a higher risk of being unemployed due to low educational attainment. Unemployment has ripple effects which include poorer health outcomes (higher depression, anxiety and self-esteem), precarious housing situations and less social networks.
Given that migrants mainly migrate for economic opportunities, policies that are integrated across the heath, labour and migration sphere should be developed to provide migrants with the opportunity to thrive.
THE RESPONSE
Migrant health has not been well researched in France. Some of the reasons behind this gap in research are said to include the lack of health statistics that include data on nationality and concerns about encouraging xenophobic or racist discourse.20 Without data on migrant health, programmatic activities and education cannot be targeted to key populations. This represents a major gap in data that should be filled as migrants are disproportionately affected by stigma and discrimination, and higher incidence of HIV in their host countries.
In 2013, France adopted a new national HIV policy where all people living with HIV are offered anti-retroviral therapy and the promotion of a “combined prevention” which links behavioral measures, testing strategies and antiretroviral therapy. Although access to HIV treatment is universal, barriers to access may still exist. These include difficulty in navigating the health care system and being denied care and treatment as a result of discrimination. France also has a higher proportion of delayed HIV diagnosis in migrants, which are likely the result of barriers to accessing health care including stigma, lack of community support, isolation, racism and double discrimination for being an HIV-positive migrant. Investing in providing targeted screening and treatment for migrants is necessary given the high incidence of HIV among migrants to France.
Founded in 2002, the Global Fund is a partnership between governments, civil society, the private sector and people affected by AIDS, malaria and tuberculosis. The Global Fund raises and invests nearly US$4 billion a year to support programs run by local experts in countries and communities most in need.
Each implementing country establishes a national committee, or Country Coordinating Mechanism, to submit requests for funding on behalf of the entire country, and to oversee implementation once the request has become a signed grant. Country Coordinating Mechanisms include representatives of every sector involved in the response to the diseases.
Algerian migrants represent the highest migrant group in France. Please click here for Algeria’s Country Coordinating Mechanism.
-SOURCES
- http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2012/dec/1650_gray_hlt_care_undocumented_migrants_intl_brief.pdf
- https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0017-4
- http://www.ces-asso.org/sites/default/files/berchet_HESG.pdf
- Desgrées du L, Pannetier J, Ravalihasy Aet al and the Parcours Group. (2015). Migrants subsahariens suivis pour le vih en france: combien ont été infectés après la migration? Estimation dans l’étude anrs-parcours // Sub-Saharan african migrants followed-up for HIV infection in France: how many acquired HIV after migration? Estimations from the anrs-parcours study et le groupe ANRS-Parcours. Journée mondiale du sida, 1er décembre 2015. http://www.invs.sante.fr/beh/2015/40-41/pdf/2015_40-41_2.pdf
- https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0017-4
- http://www.commonwealthfund.org/topics/international-health-policy/countries/france
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447687/
- http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2012/dec/1650_gray_hlt_care_undocumented_migrants_intl_brief.pdf
- http://ecdc.europa.eu/en/publications/Publications/1108_TER_HIV_in_migrants.pdf
- http://ecdc.europa.eu/en/publications/Publications/assessing-burden-disease-migrant-populations.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3901314/
- http://www.migrationpolicy.org/research/slow-motion-labor-market-integration-new-immigrants-france
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036007/
- http://www.worldometers.info/world-population/france-population/
- https://www.iom.int/world-migration
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4224795/
- http://www.unaids.org/sites/default/files/country/documents//FRA_narrative_report_2014.pdf
- http://www.unaids.org/sites/default/files/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/FRA_narrative_report_2014.pdf
- Hernando V, Arco D, Alejos B. (2015). HIV Infection in Migrant Populations in the European Union and European Economic Area in 2007–2012: An Epidemic on the Move. J Acquir Immune Defic Syndr ;Volume 70, Number 2, October 1, 2015.
- https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0017-4